A HIV-Positive Man with Ascites: Discussion
How would you interpret the immunophenotype of the abnormal cell? What are the important positives and negatives?
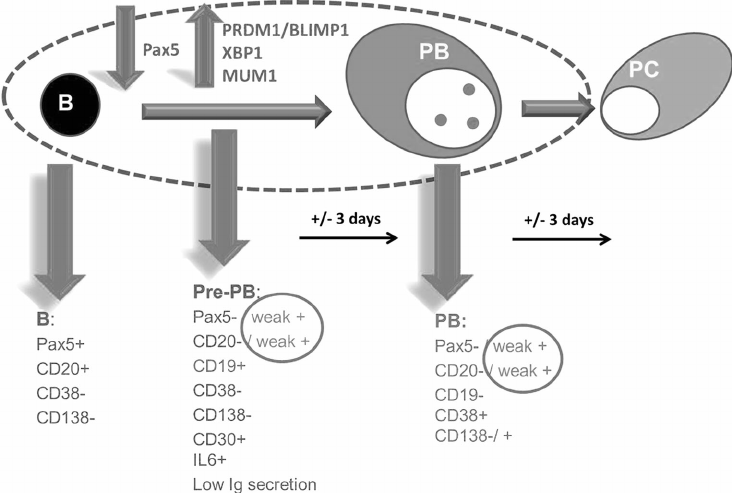
The abnormal cell is positive for CD79A, but negative for CD20 and PAX-5. CD79A expression precedes immunoglobulin and CD20 expression on B cells, and disappears later than CD20 in the late stage of B cell differentiation. It is therefore useful in distinguishing early B-cell neoplasms (such as precursor B-ALL) and plasma cell neoplasms, which are often characterised by the presence of CD79A and absence of CD20 (Chu et al., 2001).
The cells are also positive for CD38, CD138 and heterogeneously positive for CD56. The co-expression of CD38 and CD138 is characteristic of plasma cells; malignant plasma cells are often characteristed by the aberrant expression of CD56 (Robillard et al., 2014).
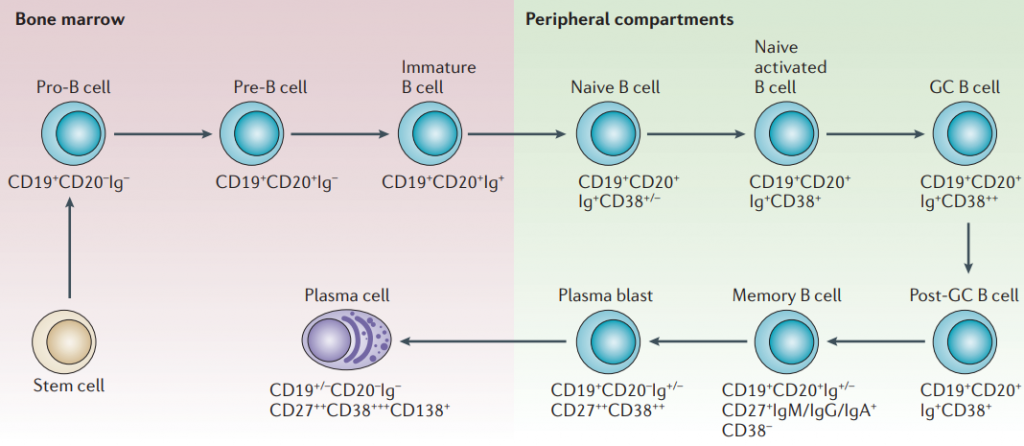
Normal B cell development. Image Source.
What is the diagnosis?
The differential diagnosis includes:
- Plasmablastic lymphoma
- Primary effusion lymphoma (goes against: HHV-8 negative, CD45 dim)
- Immunoblastic DLBCL (goes against: CD138 positive, CD20 negative)
- ALK-positive DLBCL (goes against: CD138 positive, CD20 negative)
- EBV+ DLBCL of the elderly (goes against: CD20 negative)
- Plasmablastic / anaplastic myeloma / multifocal plasmacytomas (goes against: EBER positive, malignancy in a patient with HIV/AIDS)
The diagnosis is hence likely to be plasmablastic lymphoma. A recent review (from 1997-2014) of plasmablatic lymphoma found the following selected pathological features of PBL:

The typical immunophenotype of a plasmablast (source: Boy et al., 2015)
How would you treat this patient?
Plasmablastic lymphoma is rare with a poor prognosis. The median overall survival has been reported to be 15 months in HIV-positive patients (Castillo et al., 2008). There is currently no standard of care. A small study of three patients with plasmablastic lymphoma (two HIV-positive and one negative) reported durable complete reponses to bortezomib in combination with dose-adjusted chemotherapy (V-EPOCH, Castillo et al., 2015). CODOX-M-IVAC (Magrath et al., 1996) and HyperCVAD (Cortez et al., 2002) have all been used to treat plasmablastic lymphoma. A meta-analysis of AIDS-related malignancies showed improved complete response rates when R-EPOCH was used, compared to R-CHOP (Barta et al., 2012). However, the extrapolation to plasmablastic lymphomas is difficult because of the lack of expression of CD20.
Regardless of the choice of chemotherapy regimen, this patient requires re-institution of HAART, which has been shown in a meta-analysis to improve complete response rates in AIDS-associated lymphomas (Barta et al., 2013).
