This self-assessment is intended to help new haematology trainees identify haematological emergencies and guide immediate management.
Question 1
A 48-year-old female is brought to the Emergency Department with fever. She was found unresponsive by her family members. She had been complaining of a headache and tiredness over the last few days. She has no past medical history of note. On arrival in the Emergency Department, she is confused. The FBC shows Hb 8.1 TW 8.9 Plt 18.
Toolbar
Adjustments
Brightness
Contrast
Saturation


Report the peripheral blood film.
Microangiopathic haemolytic anaemia with numerous schistocytes (>2 per high powered field, also known as RBC fragments) and polychromasia. Genuine thrombocytopaenia with no platelet clumps.
Give your differential diagnosis for the features seen on the blood film. What is the most likely diagnosis?
- Thrombotic thrombocytopaenic purpura (most likely diagnosis as there is no other obvious cause)
- Haemolytic uraemic syndrome or atypical haemolytic uraemic syndrome
- Pregnancy
- Malignancy
- Disseminated intravascular coagulation
- Hypertensive emergency (malignant hypertension)
- Drugs (e.g. gemcitabine, quinine, calcineurin inhibitors)
- Autoimmune disease
- Catastrophic antiphospholipid syndrome
How would you manage this patient?
- Take samples for ADAMSTS13 activity and antibody detection prior to initiation of plasma exchange (but do not delay plasma exchange while waiting for this result).
- Plasma exchange with 1-1.5 plasma volumes of FFP.
- Plasma volume (L) = 0.07 x weight (kg) x (1 – haematocrit)
- Alternative rule of thumb: 1PV = 40ml/kg
- Immunosuppression with prednisolone (at least 1mg/kg) or pulsed methylprednisolone (1g/day x3 days).
- Document clear advice not to transfuse platelets without prior discussion with Haematology or unless there is life-threatening bleeding.
- Thromboembolic prophylaxis: aspirin once platelets >30 and prophylactic LMWH (enoxaparin 40mg daily) once platelets >50.
- Folic acid supplementation.
- Investigations to rule out a secondary cause can be undertaken in parallel, but should not delay initiation of PLEX.
Question 2
A 31-year-old male presents to the Emergency Department with a severe headache. He is found to be pancytopaenic with Hb 9.1 TW 0.9 Plt 6.
Toolbar
Adjustments
Brightness
Contrast
Saturation


Report the peripheral blood film.
- Circulating promyelocytes with a bilobed, hypergranular appearance.
- Pancytopaenia with neutropaenia and genuine thrombocytopaenia.
What is the diagnosis?
How would you manage this patient?
- Immediatly start all-trans retinoic acid (ATRA) 45mg/m2/day in two equally divided doses. Do not wait for diagnostic confirmation to start ATRA. It must be started immediately on suspicion of APML.
- Check fibrinogen, prothrombin time (PT) and activated partial thromboplastin time (APTT) urgently.
- Correct coagulopathy and low platelets – this is essential as early mortality from APML is attributed to bleeding and APML has an overall survival of over >95% if treated optimally.
- Keep platelets >30 (>50 if bleeding, >100 if the bleeding is intracranial).
- Keep fibrinogen >1 (>1.5 if bleeding).
- Given the presentation with headache, an urgent CT brain is indicated to rule out a spontaneous intracranial haemorrhage.
- Confirmatory test: PCR to look for PML/RARA fusion oncogene or cytogenetics to look for t(15;17).
If he had presented with a TW of 400×109/L, would you consider leukopheresis for him?
No. Leukopheresis is contraindicated in APML as it can worsen the coagulopathy and bleeding.
Question 3
A 47-year-old male is brought to the Emergency Department with fatigue and breathlessness. He is tachypnoeic with an SpO2 of 86% on room air. He is also complaining of a headache. FBC shows Hb 6.9 TW 310 Plt 9.
Toolbar
Adjustments
Brightness
Contrast
Saturation


Report the peripheral blood film.
- Numerous circulating blasts with open chromatin and prominent nucleoli. Blasts do not contain Auer rods.
- Two populations of blasts:
- Medium-sized myeloblasts blasts with a high nuclear : cytoplasmic ratio, weakly basophilic cytoplasm and regular nuclear contours.
- Large blasts with more copious blue-grey cytoplasm and occasional vacuolation. These are likely monoblasts. Circulating promonocytes with folded nuclei and indistinct nucleoli are also seen.
- Genuine thrombocytopaenia with no platelet clumps.
What is the most likely diagnosis?
His chest radiograph is shown below. How would you manage him?
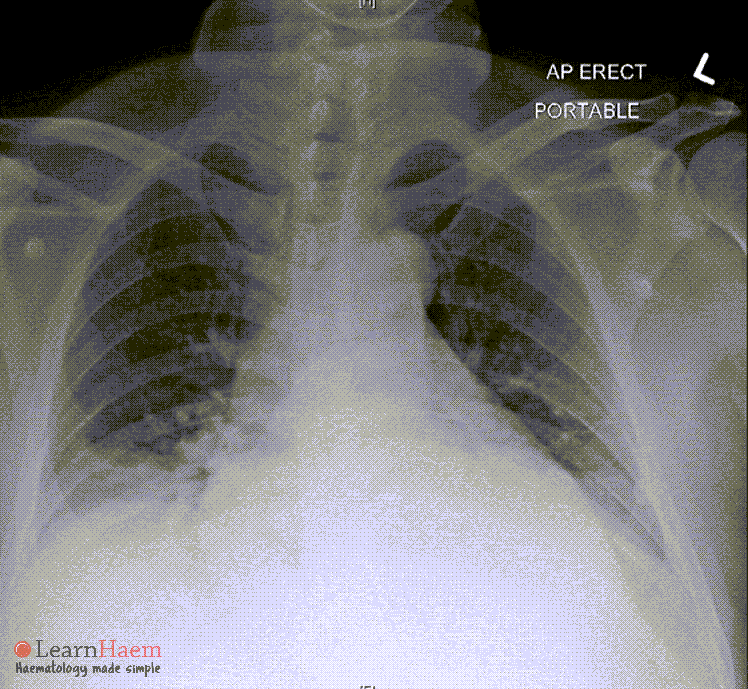
- This patient has AML with symptomatic leukostasis. Leukostasis is conventionally defined as occuring when the WBC exceeds 100×109/L, but it may occur at lower WBC, especially if blasts are large (e.g. monocytic leukaemias). Features of leukostasis include:
- Respiratory: dyspnoea, hypoxia, diffuse alveolar haemorrhage, respiratory failure.
- Central nervous system: confusion, somnolence, dizziness, headache, delirium, reduced consciousness levels, neurological deficits.
- Eye: impaired vision, retinal haemorrhage.
- Ear: tinnitus.
- Cardiovascular: myocardial ischaemia / infarction, limb ischaemia, renal vein thrombosis, priapism.
- Urgent cytoreduction is required. Cytarabine can be used for this purpose. Hydroxyurea may be used as an adjunct, but cytotoxic chemotherapy is the mainstay of treatment.
- Leukopheresis can be considered, but the evidence for this is conflicting as studies (largely of poor quality) have failed to show survival benefits with leukopheresis.
- The patient should be hydrated and adequate tumour lysis prophylaxis given.
- If transfusion is not deemed clinically urgent, it should be delayed to avoid exacerbating the hyperviscosity.
Question 4
A 84-year-old female is referred for fever, weight loss and pancytopaenia. She has a history of chronic renal disease and is on amlodipine and a thiazide diuretic for hypertension. Her last creatinine was 203 (eGFR 20). Hb 8.2 TW 2.5 Plt 33. She underwent a bone marrow aspiration and trephine biopsy. The bone marrow is shown below.
Toolbar
Adjustments
Brightness
Contrast
Saturation


What is the most obvious abnormality?
The bone marrow is infiltrated by atypical lymphoid cells with deeply basophilic cytoplasm, open chromatin, prominent nucleoli and vacuoles. The appearance is concerning for Burkitt lymphoma.
She is started on prednisolone. That evening, she complains of palpitations and tingling in her fingers. The nurse reports that she has been anuric for 12 hours. What is the most likely diagnosis and how would you investigate?
- Her symptoms are concerning for tumour lysis syndrome.
- Check her renal function and electrolytes.
- Do a 12-lead ECG.
Her lab results and ECG are shown below. How would you manage her?
Sodium 145 mmol/L (135-145)
Potassium 6.7 mmol/L (3.5-5.0)
Bicarbonate 14 mmol/L (22-31)
Anion gap 17 mmol/L (10-18)
Urea 39.5 µmol/L (2.5-7.5)
Creatinine 394 mmol/L (60-107)
Calcium 1.49 mmol/L (2.15-2.55)
Phosphate 2.95 mmol/L (0.85-1.45)
Magnesium 1.06 mmol/L (0.75-1.07)
Uric acid 831 µmol/L (220-540)
Albumin 29 g/L (38-48)
Bilirubin 14 µmol/L (5-30)
AST 48 U/L (10-50)
ALT 18 U/L (10-70)
ALP 97 UL (40-130)
LDH 8679 U/L (250-580)
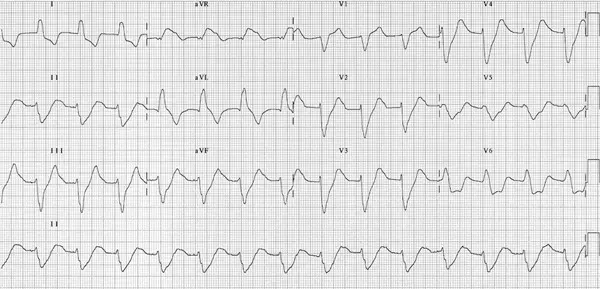
- Give rasburicase (0.2mg/kg/day is the labelled dose for high-risk patients. Prophylaxis with repeated single doses of 3mg (off-label) can be considered).
- Intravenous insulin and dextrose.
- Intravenous calcium gluconate is recommended for myocardial stabilisation given ECG findings (in TLS, the recommendation to avoid calcium replacement in asymptomatic hypocalcaemia is to avoid precipitation of calcium phosphate).
- Urgent nephrology consult for consideration of haemodialysis. This is key as she is anuric. The management otherwise usually relies on maintenance of a high urine output with vigorous hydration and careful monitoring of fluid balance.
What are the risk factors for tumour lysis syndrome?
- High tumour burden.
- Aggressive tumours with rapid cell turnover (e.g. acute lymphoblastic leukaemia, aggressive lymphomas such as Burkitt lymphoma, small cell lung cancer).
- Pre-existing renal impairment or renal involvement by tumour.
- Increased age.
- Treatment with highly active, cell-cycle specific agents.
- Concomitant use of drugs that increase uric acid levels including alcohol, ascorbic acid, aspirin, caffeine, cisplatin, diazoxide, thiazide diuretics, adrenaline (epinephrine), ethambutol, levodopa, methyldopa, nicotinic acid, pyrazinamide, phenothiazines and theophylline.
Question 5
A 28-year-old female presents with a cough which has been persistent and worsening over the last 2 months. On examination, there is facial swelling and plethora. FBC shows Hb 10.2 TW 82 Plt 34.
Toolbar
Adjustments
Brightness
Contrast
Saturation


Report the peripheral blood film.
- Circulating blasts which have a high nuclear : cytoplasmic ratio, open chromatin, weakly basophilic cytoplasm, irregular nuclear contours and occasional, indistinct nucleoli.
- Genuine thrombocytopaenia with no platelet clumps.
What investigation would you advise the managing physician to perform next?
- Chest radiograph to look for a mediastinal mass.
- CT thorax to look for evidence of airway or SVC compression / obstruction.
The patient’s chest radiograph is shown below. What is the most likely diagnosis?
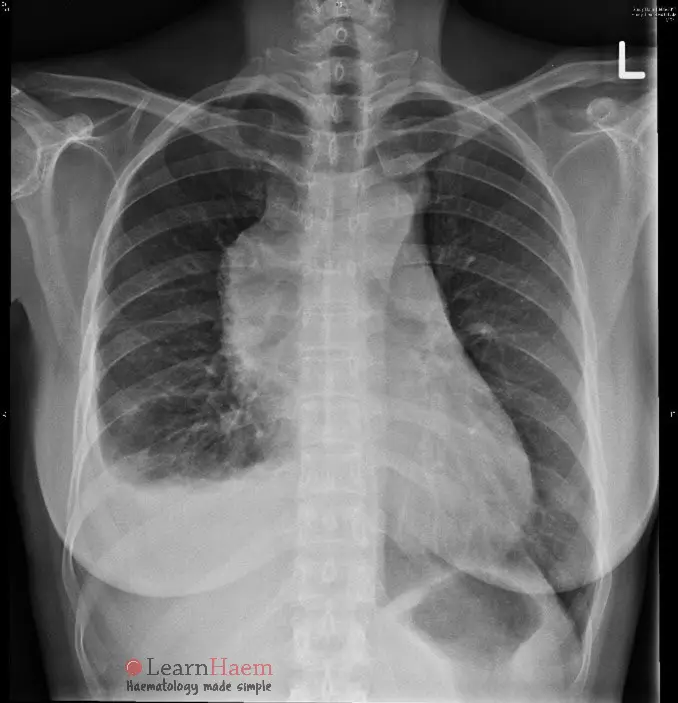
T-ALL (acute lymphoblastic leukaemia). This is one of the differential diagnoses of a mediastinal mass. If bone marrow blasts account for <25% of the total nucleated cell count, then the diagnosis is T lymphoblastic lymphoma.
How would you manage the patient?
- Nurse upright at 45°C to prevent compression of the mass on the great vessels and heart. She should never be placed prone as it has the potential to result in cardiac arrest.
- This patient should have the diagnosis confirmed with peripheral blood immunophenotyping and risk assessment done from the peripheral blood. An anterior bone marrow aspirate is possible, but given the number of circulating blasts, the diagnosis can be made on the peripheral blood.
- For patients with a normal peripheral blood film the most urgent procedure to arrange is a biopsy of the mediastinal mass. This should be done by an experienced surgeon, under local anaesthesia insofar as is possible. The patient may require standby extracorporeal membrane oxygenation (ECMO) in case conversion to general anaesthesia is required.
- Although there is compression of the trachea, this patient should not be intubated if there is no emergent indication without first consulting anaesthesia. Sedation risks loss of smooth muscle tone, with consequent airway and cardiovascular collapse. In addition, the mass is around the level of the carina on CXR. Intubation will not bypass the obstruction.
- Although there is clinical SVCO, both SVC stenting and radiotherapy are lower in priority compared to obtaining a histological diagnosis. This will allow definitive treatment to be started.
- Once the enough samples have been taken for diagnosis, steroids should be started emergently.
- Remember that if there is complete SVCO, then venous access should be obtained in the lower limbs.

no CXR loaded for q3
Hi Natasha! Sorry to hear the CXR image did not load on the page. We are unable to replicate the issue. Can you share more details – e.g. device you are accessing from and also the network (WiFi/Data) that you are using?
Thanks a lot
This is very helpful 🙂