- Cold agglutinin disease is an immune-mediated haemolytic anaemia typically characterised by complement-mediated haemolysis.
- Clinical manifestations include acrocyanosis, Raynaud phenomenon or symptomatic anaemia.
- Cold agglutinins may be non-specific and must be distinguished from CHAD.
- Screening test: incubate patient plasma with saline-suspended normal red cells for 30-60 min at room temperature. If no reaction, the cold agglutinin is not clinically-significant.
- If the test is positive, then the titre and thermal amplitude will need to be established to determine if it is clinically-significant (usually more than 30°C).
- CHAD usually has a high-titre antibody (>1:500 at 4°C) and a high thermal amplitude (>=30°C).
- Cold agglutinin disease:
- Polyspecific DCT is usually positive for C3.
- Antibody is usually anti-I (for post-infectious cold agglutinin disease, the antibody usually has anti-i specificity).
- Serum electrophoresis (keep serum sample at 37°C until serum has been separated to prevent antibody from binding to red cells) to look for monoclonal IgM.
- Consider bone marrow aspirate and trephine biopsy to look for evidence of clonal B cell disorder.


0 x
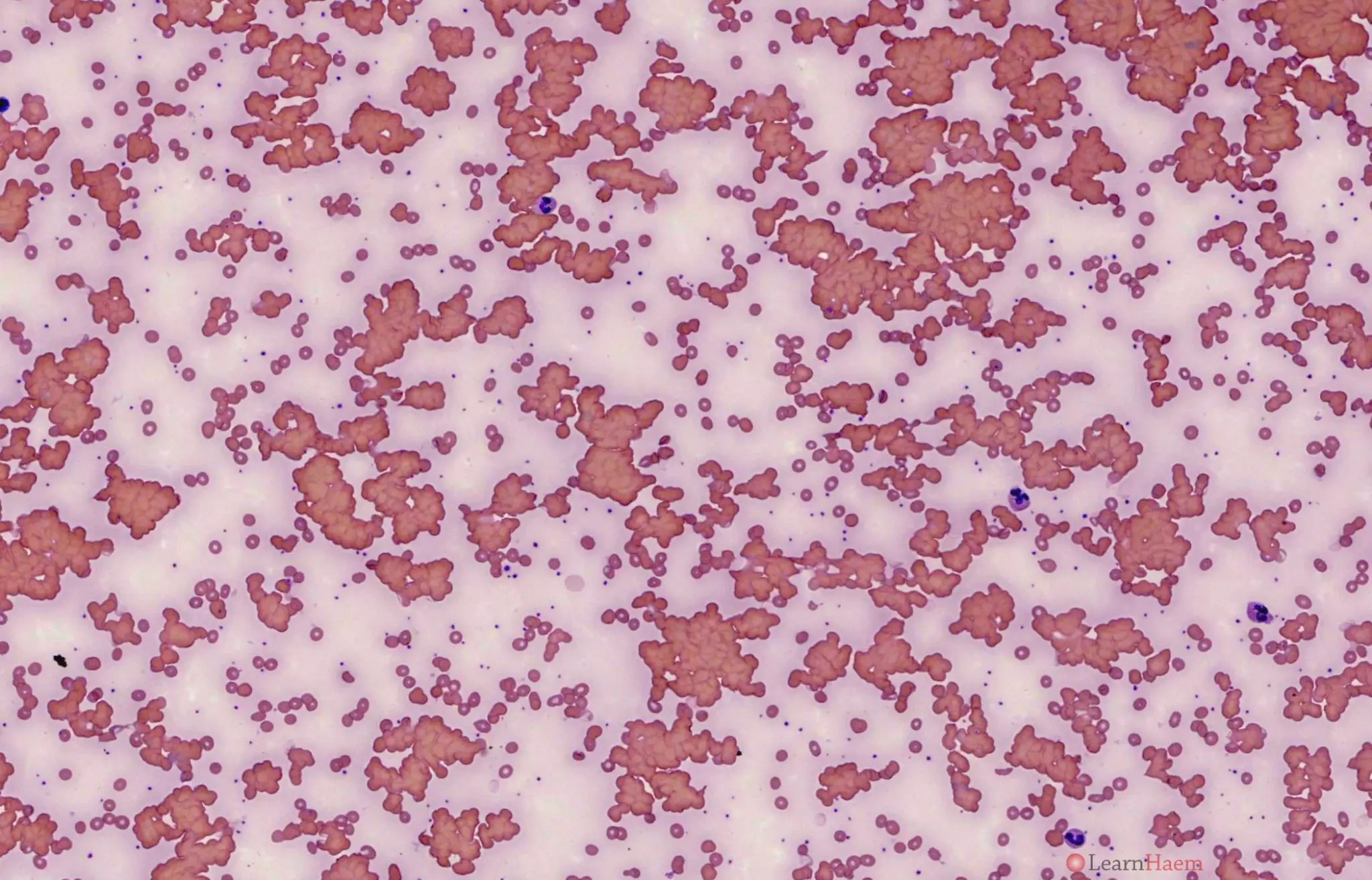
Blood film of a patient with cold agglutinin disease before warming.


0 x
Blood film of a patient with cold agglutinin disease after warming to 37°C. Note the numerous atypical lymphoid cells.


0 x
Bone marrow of the patient showing infiltration of the marrow by a mature lymphoid population.
Blood film features:
- Red cell agglutination which resolves / improves on warming to 37°C
- Spherocytes
- Polychromasia with polychromatic macrocytes
Other features to look for:
- Atypical lymphoid cells
- Rouleux
Causes:
- Primary
- Secondary
- Malignancy (especially indolent B-cell lymphomas)
- Infections (Mycoplasma pneumoniae, Epstein-Barr virus)
- Autoimmune disease

Leave A Comment